What's wrong with glaucoma drops to reduce the pressure? She wrote later on December 10, 2012:
Here is Case History No. 1536 as an example of how Dr. Kaisu has treated patients who came to her
after so-called successful operations, but without appropriate adjustment to their lenses.
There are many more examples from Dr. Viikari's case work in this book. It is literally a treasure trove
of information about treating eye patients. Especially important is the cases involving migraine headaches
which she was able to relieve by adjusting the patients's eyeglass prescriptions. People came to her from all over
Europe for relief from persistent and often un-treatable cases of migraines, and she says that she treated
over 2,000 such cases in her surgery (doctor’s office) in Turku, Finland.
In a July 22, 2011 email Dr. Viikari wrote me, "Contact lenses are the death of all relaxation of the
ciliary cramp. They are a straitjacket!" Do you remember wearing eyeglasses and taking them off for a few minutes to "rest your eyes"? Can't do that with contact lenses, can you? I recall my own reactions to wearing contact lenses prompted me to
discard them quickly. When Lasik surgery came around, I was skeptical as to its efficacy, and Dr. Viikari's
advice was to avoid it. From reports of several of our children who have had the expensive Lasik surgery
and are now unable to see clearly without glasses, I am glad I skipped that surgery. Instead, based on Dr.
Viikari's recommendations, I began wearing +D lenses (aka reading glasses) and discarded my -2D lenses.
Within 3 months, I could drive and read street signs during daylight hours without any corrective lenses. I
use +.5 D lenses while working on my computer screens, +2D for reading, and for night driving, I use -1D
lenses.
Albert Einstein once said, "Unthinking respect for authority is the greatest enemy of truth." He was not
derogating authority per se, only a respect which disengages one's own thinking ability, a respect which is
followed blindly in pursuit of monetary goals, instead of a pursuit of truth in general and the pursuit of
patients' well-being in particular, as Dr. Viikari did during her lifetime work in research and patient
treatment. Unfortunately, those journal authorities who denied her work's publication(3) have done a great
disservice to the thousands upon thousands of patients in the world who are unknowingly mistreated with
eye operations, drugs, lasers, contact lenses, etc.
Many people must wonder how the solution to the problem of ocular
accommodation, such a complicated problem, could have ever been revealed to an
eye practitioner seeing patients in a small surgery in Turku, Finland. To grasp
how this is possible, one must study the woman herself, Kaisu Viikari.
To study and understand the dynamic problems of accommodation required a
researcher with a Medical Degree in Ophthalmology, a Ph. D. in Ophthalmology,
plus these prerequisites:
- an open mind
- a totally focused person, one devoted to this one task
- someone free from providing income for her family
- someone who had mastered the basic knowledge
contained in the existing elementary textbooks about
accommodation, e.g.. those of Kaisu's father's time
[Axenfeld(4), Walsh(5)], the good times of natural eye care,
the times before mankind entered the modern age, when
children as early as 3, 4, 5 years old are
reading small text on the
screens of their Smartphones and Pads up close and without plus correction!
People have already for decades since Kaisu's original work been occupied with
their own scientific interests, e.g., medicine, astronomy, archaeology, space, air,
water, ecology, etc., and experiencing a demand to produce something. This
demand can prevent a decades-long dedication to a scientific and medical
problem, a dedication which is required for solving the mystery of ocular accommodation. Kaisu Viikari has given this dedication and solved this problem, and yet scientists still claim there is no solution. They continue to look in the dark
of their academies, all the while, out in the open, in the light of her books, there is
the solution, waiting for the academics to absorb and learn from them, and especially for eye doctors to begin "doing no harm to their patients" as their Hippocratic Oath requires.
In addition Kaisu has been in a favorable position to study the autonomic nervous
system during her dissertation work, and appreciated the limitless importance of
the autonomic nervous system for the organism and it became clear how
important it was to solving the problem of ocular accommodation. For example,
understanding how positive accommodation affects the parasympathetic nervous
system and de-accommodation (i.e., relaxation of the accommodating muscle m.
ciliaris, which can also be voluntary) affects the sympathetic nervous system.
Dr. Kaisu Viikari could
have had no idea how much the research she documented in her dissertation and early books (such as this one) would "rock
the boat" of academics in her field of ophthalmology in future decades! Only now, retired from her daily work of seeing patients in her
small office, can she devote time to correcting the numerous injustices done to her work by
academics who rail against her work in the absence of any signs of their having
studied, much less having understood, her work. [See her book,
The Struggle for details of these injustices.)
At the age of 92, she has mastered the Internet and emails enough to help set the
record straight about the ease and simplicity of the corrections needed to save the
eyes of people, especially children, from the ravages the technology in the 21st
Century can create upon their eyes and overall health.
On June 27, 2014, I received this correspondance and have edited it slightly for this review. It is a precise and concise description of how accommodation strain can be transmitted via the trigeminus nerve to create pain in all sections of the human body.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Accommodation and the Trigeminus nerve
by
Dr. Kaisu Viikari, Ph. D., M.D. Ophthalmology
A Personal Correspondance
Translated from the Finnish by Liisa Honkasaari
In my earlier writings, I made reference to a highly important topic — the way
accommodation strain is reflected to our entire bodies. This is made possible by the extensive,
tree-like structure of our nervous system, in which everything is connected to everything else. For
example, communicating branches (rami communicantes) link the major subsystems of the
peripheral and the autonomic nervous system from the nerves in the spinal cord to the
sympathetic trunk and vice versa. Almost any impulse may thus be projected to any part of our
bodies.
For example, researchers are well familiar with the concept of referred pain, where pain is
felt at a location far away from the actual process causing it. While you may come across
textbooks of ophthalmology that mention referred pain symptoms related to accommodation,
they appear to pass them by with only a cursory discussion, judging from the fact that in practice,
you very rarely see this highly important, extensive, and extremely central area of medicine being
applied in treatment. Quite commonly, the aim seems to be at the "best visual acuity", which is
hardly a sound basis for treatment of the whole human, as it focuses only the acuity of the eyes
which may be achieved at the expense of the health of the eyes and the rest of the body.
A fogging examination will illustrate these referred pain neurophysiological phenomena in
more concrete terms in a human being. It has happened several times that a co-operative patient
of mine, under strong fogging of a number of dioptres, suddenly cried out: "What an awful shock
wave went through me, all the way to the tips of my toes!" or "Goodness, I just cannot keep my
eyes open, it's like my eyes were being pricked by a thousand needles!" The fogging had caused
a massive release in the accommodation muscle, which triggered such a strong impulse in its
nervous branches that it went through the entire network of the nervous system and the body.
Any doctor who has witnessed this physical reaction, which I have on many occasions, cannot
deny the effect that a narrow mindset focused primarily on visual acuity may have on the health of a patient.
Of all of our physiological functions, accommodation strain is perhaps the one that is most
widely shared by us modern humans, and the work of the accommodation muscle, apart from the
heart, perhaps the most ceaseless. Stress on our eyes thus often is the final straw that causes an
upheaval in our bodily resources. However, while releasing accommodation strain is an
extremely easily implemented and rewarding therapeutic intervention, it is a great loss to all
peoples of this world that it is not exploited as fully as possible, up until now.
If the physiology of accommodation and the significance of accommodation strain are not
fully understood, the examination of the cause at the root of the patients' problems, or etiology, is
misdirected, being based on wrong assumptions, and the treatment becomes hit and miss. This is
even more regrettable as the trigeminal nerve (Nervus trigeminus), a vital sensory nerve in our
bodies named as the cause of the most infernal pain, is also the sensory nerve for the eye, and it
plays an important neuro-ophthalomological role.
Anatomy
The trigeminus nerve, or V-cranial nerve, whose name describes its three branches, starts
from a nucleus located in the brain, in the pons in the base of the skull. Morphologically, it is
closely associated with another important nerve in the eye, or the oculomotor nerve (N.
oculomotorius, III cerebral nerve). On its way to the eyeball, it sends a so-called long branch to
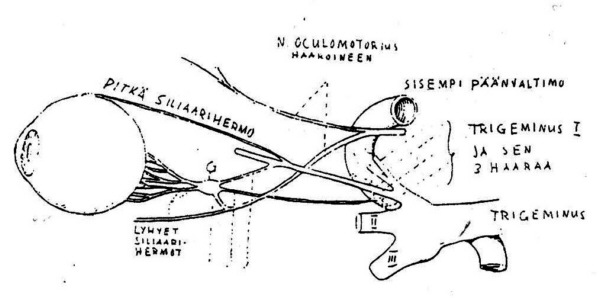
the ganglion ciliare at the back of the eye socket(Figure 1).
Despite of its small size, only a couple of millimetres, this ganglion is highly important, both
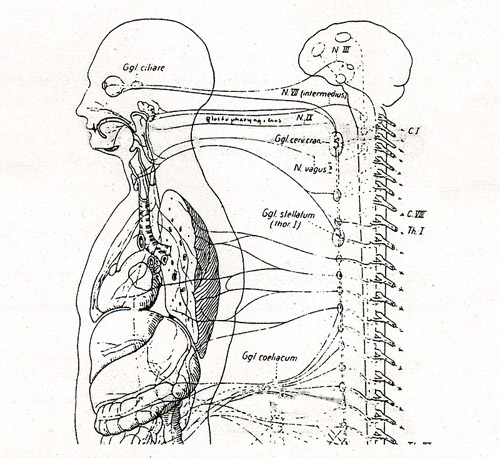
anatomically and physiologically. Figure 2, which shows how the nerve tracks from ggl. eiliare
connect like reins with the rest of our tree-like nervous system, is intended to support the
permanent memorisation of this vital centre's location.
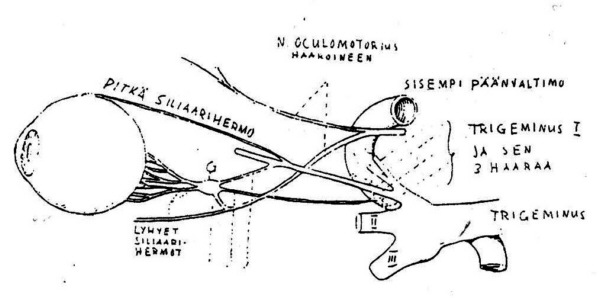
Figure 1. Ciliary ganglion G = Ganglion ciliare, 1 = root of the parasympathetic oculomotor
nerve (Nervous ocumolorius) 2 = root of the sympathetic nerve plexus 3= root of the trigemenial
nerve (Nervus trigeminus).
Figure 2 An illustrative figure showing the
location of the ganglion ciliare and nervous
tracks that, like reins, connect this important
ganglion to the entire tree-like nervous
system in our bodies.
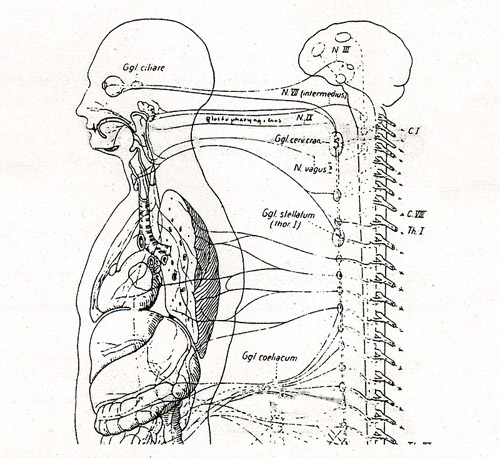
How clearly this image reminds me of the way
in which almost every migraine patient,
when describing where they feel the pain,
presses their fingers on the location of that ganglion on their temples, on one side or the other,
sometimes on alternating sides, or on both sides simultaneously. I have also personally
experienced the "knife stab" at the back of the eyeball from the time when I used to stay up all
night writing my thesis for the first and the last time, as nowadays I continuously wear my
plus glasses!
Branches from cranial nerve III and from the sympathetic nerve plexus surrounding the carotid
and cranial arteries also extend to ganglion ciliare, this meeting place for the various components
of our nervous system.
From the front of the ganglion ciliare, the nerve fibres continue on and divide into some twenty
branches and (as short ciliary nerves) go through the eyeball together with the optic nerve (N.
opticus, cranial nerve II), then travel between the coats lining the eyeball and reach the front
sections of the eye, the ciliary muscle, the iris and the cornea.
Figure 1 further shows how two branches of the trigeminal nerve travel along both sides (as long
ciliary nerves), also to the front of the eye. The cornea was designed to provide efficient
protection for the eye. Consequently, here the nerve branches into numerous end organs, with
more or less one for each surface cell. Indeed, the cornea is the part in our bodies that has the
highest density of sensory nerve endings, which explains the "thousand needles" I mentioned
earlier.
The optical branch of trigeminus I (N. ophthalmicus) also sends filaments to the external
muscles of the eye, which should be remembered when patients sometimes, for example when
suffering from flu, complain about sensitivity when moving the eyes.
When we accommodate our eyes, resulting in overstrain in the accommodation muscles, this
means that the ciliary muscle is overstrained and feels it as discomfort, similarly to any other
muscle. The trigeminus nerve then transmits this pain not only to the eye and its surroundings but
also other parts of the body. I wonder how many doctors in general realise that their patient's
headache is caused by the trigeminus nerve!
It should be possible to get a reasonable idea of the many and varied trigeminus symptoms
from proper text books, but to my own eyes it was revealed specifically when examining my
extensive body of migraine patients with severe symptoms (some 2,500 cases), and the
symptoms I discuss here all belong to the same category.
I write down an accurate anamnesis (medical history), however, without leading the patient,
as the patient's own expressions are invaluable. With accurate correspondence to anatomical
innervation zones, the patients then describe a huge variety of symptoms. I thought I had already
heard it all when, as I was planning this article, a 38-year-old woman (P.H.) described her
headache as follows: "It feels like somewhere inside my head, in the middle of the brain,
somebody was pushing up a sharp wedge, the sides of which tend to widen and cause a feeling of
pressure." I would possibly associate this with the branch of trigeminus I leading to the brain,
which innervates the tentorium part of the hard meninges (Tentorium cerebelli).
In general, a number of sensory branches lead to the neurocranium, not only from all three
branches of the trigeminus (rami meningici) but also from cranial nerves X and XII. These
explain why an ache caused by the eyes may be felt in all areas of the head, often even as a band
around the head, which is not at all obvious to the patients. On the contrary, when I suggest that
their headache could be caused by the eyes, their usual argument is, "But I feel it at the very back
of my head!"
In addition to aches in the actual eye and its immediate surroundings, the forehead is one of
the most usual areas where pain is felt. The said branches of the trigeminus nerve exit the skull
via the upper edge of the eye socket, then turn up towards the forehead and top of the head. Some
patients may say their scalp is so sensitive they cannot comb their hair. Sensitivity may be felt at
the "holes" in the upper edge of the eye socket, and rubbing these spots feels good and provides
relief. This is one area, in addition to spots corresponding with many other branches of the
trigeminus nerve in the face, that Chinese school children are taught to massage to release
accommodation in an effort to prevent myopia.
Sneezing
The "funniest" symptoms are those produced by the neural endings of trigeminus II that
extend from above and back to the nasal mucous membranes. To promote the release of the
accommodation spasm so that I can examine refraction, I usually make (headache) patients wait
for some time, wearing plus glasses that release the cramp (or "confiscate" their minus glasses).
At times, after a while, I hear an extraordinary burst of sneezing from the waiting room, and the
patient calls out from behind the door: "It's because of these glasses!" "I know", is my reply.
When the tightly contracted accommodation muscle is suddenly released, such a strong
impulse in the trigeminus nerve is caused that it triggers the sneezing reflex. I know from
personal experience how, when you spread out your newspaper in the morning, you can
sometimes start sneezing in a similar fashion, the more readily, the more under-corrected glasses
you are wearing. Patients often think this is caused by an "allergy to the newsprint ink"! In this
case, the accommodation muscle, which relaxes while we rest at night, suddenly has to assume
its reading tonus. This again means an exceptionally big change in the muscle, which triggers a
nervous impulse. It may also happen later on in the day if you, in the middle of your usual daily
chores, for example pick up a dictionary with small print and start looking for a certain entry,
perhaps even using the top section of bifocals.
It seems that both a major release and a contraction of the muscle are equally likely to trigger
a strong nervous impulse — in this case, in the trigeminus nerve. In an ordinary person's life,
naturally, the triggering effect usually is a contraction in the muscle.
The same mechanism is in the background of several types of runny noses caused by the
circulatory and nervous systems, or so-called vasomotoric rhinitis. The patients often afterwards
interpret them as allergies, or else they think they have caught a cold, but for some funny reason,
the illnesses progresses no further. For several years, I have had the opportunity of observing
patients of this type. It is perhaps also worth mentioning that the nasal discharge produced by
sneezing is much thicker and more viscous in its consistency than nasal discharge during an
ordinary period or, for example, tears provoked by the wind.
Phonetic sneezing
The following amusing observation, while perhaps slightly more complicated, is a similar
reaction transmitted by the trigeminus nerve:
We were attending a conference in Sidney, and the "ladies" had taken lunch at a very dimly
lit restaurant. When this group emerged to face the blinding southern sun, after a short while
there was an incredible chorus of sneezing on the street! It is possible that I was particularly
sensitive to observing it — as I had been tuned in to this issue for years.
This reflex has been explained in many ways, but my own version is the following:
naturally, there is no uncertainty about the cause, which is light. But why did not everybody react
in the same way? For example, why not I myself, even if at other times I have frequently
experienced the same phenomenon? Light triggers a strong contraction of the pupil. Knowing
that a group of women in the conference-going age is likely to wear glasses that are under-corrected in the plus direction, and as in general they do not have distance glasses with plus
sections, their pupils would already be rather small as a result of parasympaticonia caused by
accommodation strain. When a pupil like this is hit by strong light, the muscle regulating the
pupil needs to contract further. This amounts to such a major impulse in the iris that its sensory
nerve, or trigeminus, triggers a sneezing reflex. As I wear glasses with a considerable degree of
plus correction, my pupil, on the other hand, is usually not small, and it can manage the
protective action required by light with less drama.
The same explanation applies to light sensitivity that uncorrected hyperopes so often
complain about. I usually say we should see what symptoms remain after you have been wearing
normal clear glasses for a while, and then we can think about tinted lenses.
This ever wiser scientific world of ours contains an incredible number of self-evident truths,
over which there hovers an atmosphere of the great unknown! The sneezing reflex caused by
bright light is one of these. As late as in 1984, one out of maybe four of the most distinguished
medical journals in the world was wondering how this reflex is so poorly known to neurologists.
However, an article on this question can be traced back to as early as 1954(6), and Everett (1964)(7) even reports a case, a 25-year-old man, who deliberately looks into the sun to enjoy a good
sneeze!
It is such a pity that information about refraction and the glasses the patients were wearing is
lacking in these articles, similarly to all medical and even ophthalmological literature in general —
should we say, in 100 per cent of cases. In this respect ophthalmologist have done, and are still
doing, a poor job.
And yet another example of an impulse that provokes sneezing: a patient was wondering
why he always sneezes "when scratching his head"? Obviously, his nails hit a branch of the
trigeminus (triteminal nerve) responsible for enervating the top of the head. In my book, Panacea,
I also describe patients who experienced similar sneezing reflexes.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~